As President and CEO of St. Tammany Health System (STHS), Joan Coffman captains the fleet, as the health system encompasses its Covington hospital plus its supporting facilities throughout the service district. She and the fleet are now successfully navigating the uncharted waters of COVID-19’s outbreak—and she gives all the accolades to her crew. “I’m incredibly proud of the teamwork, dedication, innovation, resilience and heartfelt care our team has stepped up to provide. Here, I’d like to shine the spotlight on those working so diligently on the front lines as they share their experiences fighting COVID 19.”
On March 20, Sharon Toups found herself in line for Mandeville Diagnostic Center’s drive-by COVID testing – the first service of its kind in the parish. Ironically, as STHS’s Chief Operating Officer, she was about to be a patient at the very groundbreaking operation she was instrumental in creating.
By Day-6 of the COVID outbreak, STHS quickly developed a unique action plan for drive-through testing by coordinating necessary resources in an involved but very worthwhile undertaking. Security, Grounds staff, Patient Registration staff and others now work together in a new way with redeployed nurses, some from closed physician offices, taking specimens for the test. At its height, 40-50 patients were being tested daily, never getting out of their cars. In conjunction, a call center was established to follow-up with tested patients.
Says Toups, “I’m proud of how the team came together, and patients – including myself – are very grateful for the continuing interaction. After experiencing the process for myself, I am appreciative of it on a whole new level. It was easy, efficient and my results came back quickly. I recovered at home where Employee Health followed up with me. My 87-year-old mother also got it and was treated here at the hospital where she got fabulous care. The patient experience really hits home when it’s your own family. I know firsthand the effort and extraordinary teamwork it takes to perform under these unprecedented circumstances. Nurses and doctors come to mind first as heroes, but they can’t function without the people working in maintenance, housekeeping, radiology, labs and other clinical and support areas.”
In the weeks leading up to the crisis, STHS began careful tactical planning and commenced command center operations on March 10. Plant Operations, Grounds and Security teams set up tents outside of the Covington and Mandeville emergency departments to do triage and separate COVID patients before entering those facilities. Operations also converted patient rooms to negative pressure so contaminated air flow went out of the building instead of back into hallways. Security manned entrances to limit patient visitors. Materials Management faced shortages in securing personal protective equipment (PPE) and supplies but were creative in cultivating alternatives such as state and national resources, and securing donations of N95 masks from contractors. Inventory was centralized and prioritized with outpatient and elective procedures limited.
Toups is quick to stress the selfless contributions of supporting departments. “Environmental Services staff volunteered to do the unrelished job of suiting up to clean and disinfect support areas for COVID. To enhance their efforts, we purchased ‘the twins’ – two Solaris Lytbot UV light emitting robots to go in and further decontaminate rooms while limiting staff exposure. Food Services continues to feed patients and has taken on the role of grocery for employees working long shifts by offering milk, bread and essentials. Because ordering outside food is restricted, they adjusted their hours to ensure night and weekend workers have meals. They also coordinate food donations from the community making sure that all have an equal share in that generosity.”
Personnel were managed and maximized from the beginning, Toups explains. Security set up screening stations at entrances to prohibit any visitors or delivery persons with symptoms, or those who traveled internationally, from entering. Employees in non-use areas signed up to work entry-door shifts. And with outpatient procedures limited, staff readjusted their duties to accommodate COVID patients who have recovered but still have issues requiring such services as chest x-rays and CT scans. Lab staff were instrumental in accepting specimens for testing and worked on solutions to decrease turnaround time and eventually bring the process in-house. “It’s heartwarming to see people offering to put themselves in harm’s way for what’s best for the community,” adds Toups. “It takes all these unsung heroes here in the background making sure patients and people caring for them have everything they need.”
STHS Chief Medical Officer Dr. Patrick Torcson echoes the importance of teamwork and planning. “As of March 10, it was no longer business as usual and we had to meet the difficult challenge to shift modes.” On staff for over 30 years, he is responsible for providing quality medical care to patients and overseeing 400 physicians. “Along with escalated patient care, we focused on protecting the community.” Torcson said that watching the progression of the pandemic in New Orleans heightened concerns about a rapid increase in numbers here. “It’s helpful that people have adhered to stay-at-home orders, so we were able to slow down cases on the Northshore.” He explains that by learning from other cities, STHS went into the pandemic well-staffed and easily accommodated the patients that did come, but that there was still much to learn.
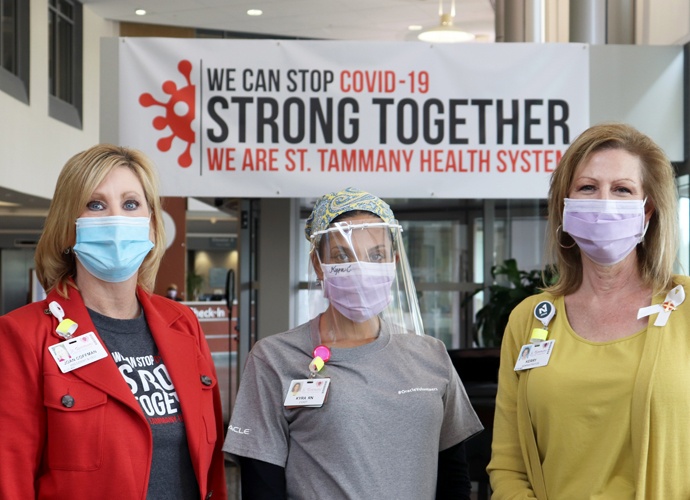
One new skill set was the proper use of PPE including a mask, face shield, hat, two pair of gloves and a gown to be worn for the duration of their 12-hour shift, including change outs between patients. He applauds the willingness of caregivers to endure heat and physical discomfort, and to learn correct procedures using the buddy system to prevent breaches. “Healthcare is a 24/7 operation and the dedication of everyone working under these conditions – their teamwork and camaraderie is very inspiring.”
For those needing inpatient care, Torcson touts the expertise of STHS’s six pulmonary critical care specialists. “Being able to treat a patient needing a ventilator is very challenging. We went to great lengths to network with specialists around the country to manage that process and to find alternative ways to support patients’ breathing. The skill of our pulmonary doctors with the sickest of patients certainly stands out.”
On why St. Tammany has fewer cases of COVID hospitalized than other parishes, Torcson says early drive-through testing is key. “By establishing our Mandeville drive-through testing site as soon as possible, we are able to give primary care doctors ways to treat their patients before they need emergency services. With this proactive testing option, physicians can get results that help with early treatment, self-quarantining and social distancing.”
The nursing staff is often considered the backbone of a hospital and as such, STHS’s Chief Nursing Officer Kerry Milton began rallying her troops well before the arrival of their first COVID patient. PPE donning and doffing were practiced, video education was presented and preparation for triage began, recognizing that throughout the country, patients were presenting in near critical to critical condition. “We needed to understand where patients could be housed; if we had enough ventilators and supplies, and how to handle an influx of patients at a fast pace. We listened to our people at nurse leader meetings to assess staffing needs and necessary skills to get ahead of it.” Some of what resulted was the creation of six-week schedule blocks covering units 24 hours a day, a communication plan that includes daily meetings with department leaders, and concise dissemination of information to staff. Care for patients who are discharged but isolated and still in need of care has been taken up by the home health department. These nurses work in patients’ homes acting as a lifeline to complete lab work and provide supplies, information and support.
“There is fear,“ says Milton, who engaged her team by personally performing rounds on all units, “but being prepared and reinforcing skills ahead of time makes all the difference.” Milton’s team was also empowered to innovate. They put forth ideas about protecting staff from airborne contaminates during the ventilation process which the building team executed by designing a plexiglass barrier placed around the patient. To prolong the life of PPE, an idea to disinfect masks in the UV machines used to disinfect Ipads was implemented. And, IV equipment was fitted with 10-foot tubing so controls could be set from outside the patient room door, decreasing exposure to staff.
Along with physical protection, STHS recognized the importance of providing resilience for staff working 12-hour shifts, 7 days straight and serving as patients’ only connection to the outside. “Almost Home” rooms were designated in surgical areas to be used at the end of shifts, providing a place to decompress, clean-up and change into clean clothes before returning to their families. “Recharge” rooms were set up with social workers, comfortable seating, snacks, a cozy atmosphere and relaxing music to help caregivers deal with the emotionally intense demands of the job.
In the most tragic of cases, it is a nurse who solely holds their dying patient with one hand while holding an Ipad in the other as family members witness from afar the passing of their quarantined loved one. “The empathy nurses give for dying patients and their families takes a personal toll,” explains Milton somberly. “It is an unimaginably difficult and heroic act of love to grant the only possibility for a final goodbye. I have the utmost admiration and respect for their service.”
Coffman, Toups, Torcson and Milton all agree that community support has been instrumental in STHS’s success and has buoyed all the staff. “Supporters coming forward with meals, homemade masks, and people offering to pray have all been very uplifting,” says Milton. The ‘Chalk Fairies,’ nurses working in the adjoining medical building, get together and write motivational messages like ‘heroes work here’ on hospital sidewalks. As their colleagues walk into work, they are filled with pride and hope.”
Dr. Torcson adds, “There’s a special quality of life here on the Northshore and our neighbors care for others, each in their own way. I particularly appreciate the focus on staying home. That’s the right thing to do. We still have a way to go before returning to a pre-COVID lifestyle, but in a spirit of resiliency, we’ll come out a stronger community on the other end.”